April 16, 2024
Tales from the Frontline:
APHA Congress 2024

Members of the Australian Private Hospitals Association (APHA) gathered in glorious weather on the Gold Coast for their annual congress last week but the industry forecast was for turbulence and storms ahead.
Across the two-day event, MediRecords Tim Pegler found that the recurring theme was that many private hospitals are barely breaking even — or are loss-making — and that hospital closures are imminent.
Mental health facilities are struggling to recruit and retain psychiatrists, who can find a better income and lifestyle working privately via telehealth. Private maternity hospitals are also at risk.
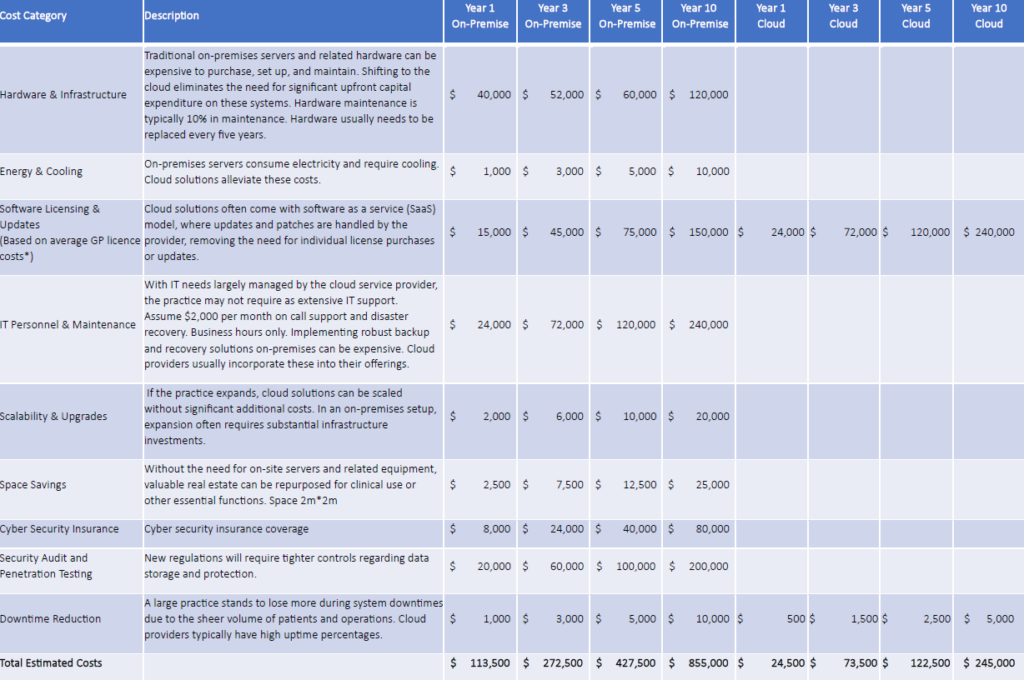
Tension with the private health insurance (PHI) industry was evident; many APHA members pointed to indexation of PHI fees failing to keep up with escalating costs for labour, IT systems, insurances, administration, cybersecurity, and building costs.
PHI representatives returned fire, being critical of private hospitals building new facilities that result in competition for doctors, which are already in scant supply. They said rising costs of living are driving consumers to downgrade their PHI memberships, making them eligible for fewer private hospital procedures.
If private hospitals close, particularly in regional areas where doctors are scarce, the impact will be felt throughout the public system with longer waitlists and more pressure on emergency departments.
An appetite to find common goals and work together – government, private sector, public sector and PHIs, seemed to be one positive note for the Congress.
Other Congress insights
- 15 private hospitals have closed in the past year, including 4 mental health facilities.
- The national shortage of GPs and radiologists is likely to worsen, with a generation of practitioners due for retirement without ready replacements.
- Private hospital operating costs are rising rapidly while revenue is falling. 43% of hospitals have an EBITDA below 5% and 68% below 10%. A consultant warned that innovation and investment are not occurring and if this doesn’t change further closures are likely.
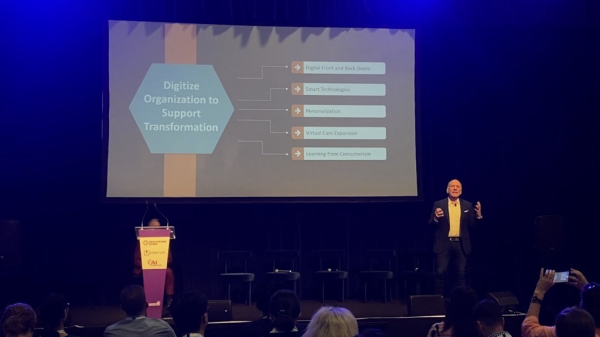
- The public system has embraced virtual care more than the private hospital system.
- Queensland Health has a Surgery Connect program outsourcing waitlisted surgical procedures to private hospitals.
- PHI representatives say chemotherapy, hospital in the home and rehabilitation in the home programs will be vital to support Australians but more GPs need to refer to these services.
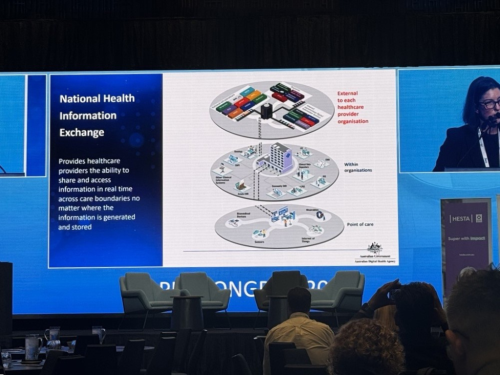
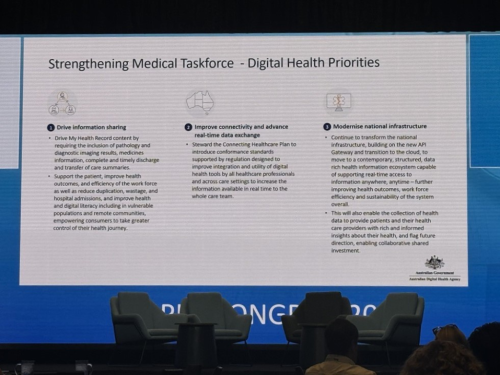
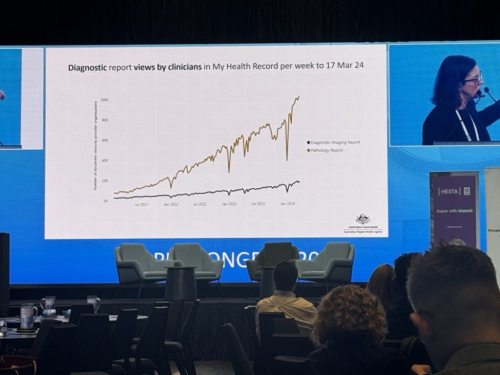
- The ADHA reported strong growth in use of the My Health Record (MHR), which now houses 50% of pathology reports and 20% of diagnostic imaging reports. It urged more private hospitals to integrate with the MHR, cautioning that disconnected health information systems “are no longer sustainable”.


![1[1]](https://medirecords.com/wp-content/uploads/elementor/thumbs/11-qms1b7uxb3sgdz5s8f2hc8iz6xweq257bqmuek6d2e.png)