The pandemic years have been actioned-packed for health-tech. What have we learned and what can we expect from 2023?
1. The cloud is (still) coming
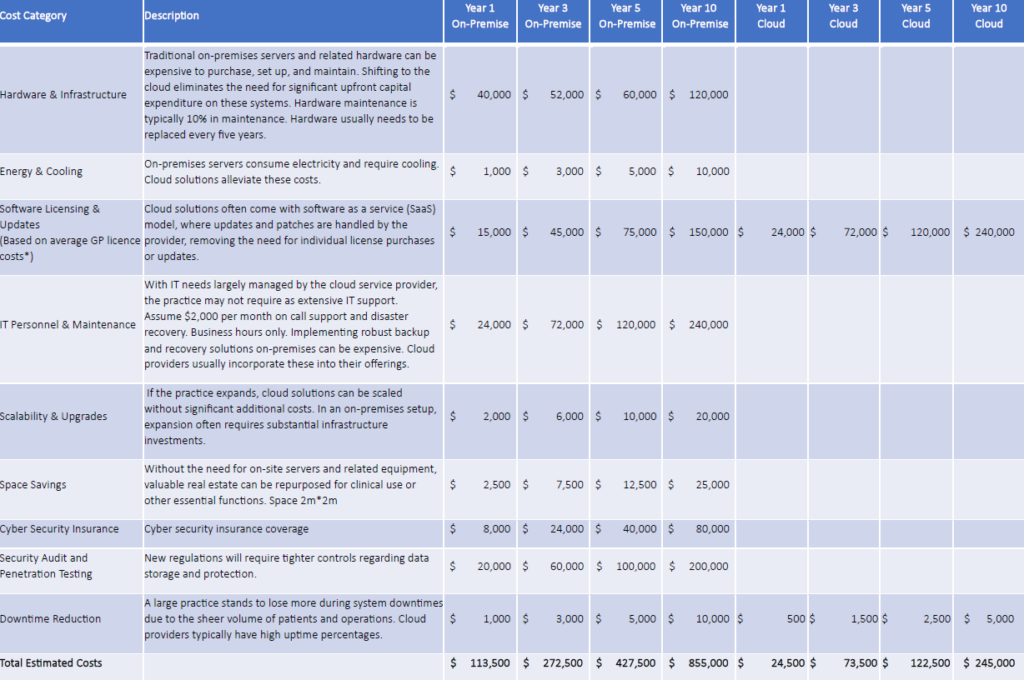
Based on conversations with customers, the market is increasingly aware of the security and infrastructure benefits of shifting to cloud. So why is the transition so slow? Partly because the healthcare industry is often understaffed, time poor and therefore change averse. The good news is that those who embrace fresh and more flexible technology rarely look back.
Speaking of shiny and new…
2. Robots are here to help
Staff shortages due to illness, burnout and pandemic-related workforce changes necessitate doing more with less. We can expect automation to play a bigger role in repetitive tasks, and robots to play support and even investigative roles.
Exhibit A: Robot dietitian RMC adds robot dietician (thetandd.com)
Exhibit B: Robot meds Mayo Clinic picks up stake in startup making pill-sized robot (beckershospitalreview.com)
Exhibit C: AI bed management NUHS’s AI platform predicts bed state 2 weeks in advance | Healthcare IT News
Exhibit D: Robot cleaning crews Cameron employs robots to super clean facilities | Heraldrepublican | kpcnews.com
The automation trend also means…
3. Lock in telehealth
Virtual and remote care are generally cheaper than hospital beds (How to implement a virtual ED in 10 weeks – Wild Health Summits : Connectivity) and more consumer friendly than queuing for in-person care (see The cost and carbon savings of telehealth, quantified (beckershospitalreview.com)). Virtual mental health care, in particular, appears to be cementing its role. However, digital literacy and equitable access to technology, including Internet coverage, can be barriers to care. Successful virtual care hinges on having accurate information, tools and help whenever needed so…
4. Maybe it’s time to make new friends
Difficulty accessing developers and tight tech budgets mean partnering can be the faster (and cheaper) path to product enhancement, in contrast to D-I-Y builds. Which means…
5. Interoperability is king
Products designed for integration have a strategic advantage over those that have not committed to interoperability at their core. Speaking the same language helps and Fast Health Interoperability Resources (FHIR) (Welcome to the HL7 FHIR Foundation) are the way to future-proof your health tech. Another interoperability truth is…
6. Clean data counts
Making sense out of a hotchpotch of data dropped into a free-text box is time consuming and painful for data analysis. Storing information in a logical, consistent and correctly coded format (MediRecords uses SNOMED CT AU SNOMED CT-AU and Australian Medicines Terminology June 2022 Release | Australian Digital Health Agency) helps the data wranglers do their thing. Quality, clean, actionable data has value and needs to be kept safe because…
7. Cyber attacks are on the rise
US data shows ransomware attacks more than doubled from 2016 to 2021 (JAMA Health Forum – Health Policy, Health Care Reform, Health Affairs | JAMA Health Forum | JAMA Network). The UK and Australia are also under siege. Minimising risk is mandatory and, while no system is risk-free, cloud technology allows you to outsource security management and those never-ending software updates so you can concentrate on core business. This is important because…
8. Change is gonna come
Australian governments are still exploring how to introduce systemic change following royal commissions into aged care and mental health services (Victoria). Royal commissions are ongoing into disability, and defence and veteran suicide. The Australian Digital Health Agency is promoting collaboration and reform. NSW is working on a Single Digital Patient Record (SDPR). Victoria is moving toward a health-information exchange system, connected to a statewide Mental Health Client Management System. Queensland is pursuing better health information connectivity and remote monitoring options. Tasmania has a digital transformation strategy underway. There are versions of virtual emergency departments emerging across Australia…
Buckle up. 2023 could be a wild ride.
About MediRecords
MediRecords is a FHIR-enabled, true cloud clinical platform with ePrescribing and telehealth integrations. MediRecords supports GP, multidisciplinary and specialist clinics across Australia and is working with Queensland Health, the Victorian Virtual Emergency Department and the Australian Defence Force on innovative models of care delivery. Please book a demo if you’d like to discuss solutions for your business.
Want to dive deeper? Further reading below:
2023 predictions: Health tech suppliers give their verdict (digitalhealth.net)
What health tech trends CIOs are focused on in 2023 (beckershospitalreview.com)
Virtual everything, asynchronous care, sustainability: Healthcare innovation predictions for ’23 (beckershospitalreview.com)
CMIOs on what to project for 2023 (beckershospitalreview.com)
Digital Health Review of the Year 2022
MR.R4.CORE\Home – FHIR v4.0.1 (medirecords.com)
Report: Telehealth accounts for about 10% of outpatient visits | MobiHealthNews
The King’s Fund interoperability report highlights relationships and tech (digitalhealth.net)
Russian hacking group ‘KillNet’ targets US healthcare (beckershospitalreview.com)
2023 forecast: 7 big-picture goals for hospital leaders (fiercehealthcare.com)
Top 10 hospital and payer trends to watch in 2023 | Healthcare Finance News
National Digital Health Strategy and Framework for Action | Australian Digital Health Agency
Digital Health Transformation – Improving Patient Outcomes 2022-2032 | Tasmanian Department of Health
DOH-Strategic-Plan-Nov-2022-update.pdf (health.qld.gov.au)
victorias-digital-health-roadmap.pdf
Single digital patient record set to deliver vastly improved patient experience | eHealth NSW